SFB 1192
Hamburg Glomerulonephritis Registry
For patients
What is the Hamburg Glomerulonephritis Registry?
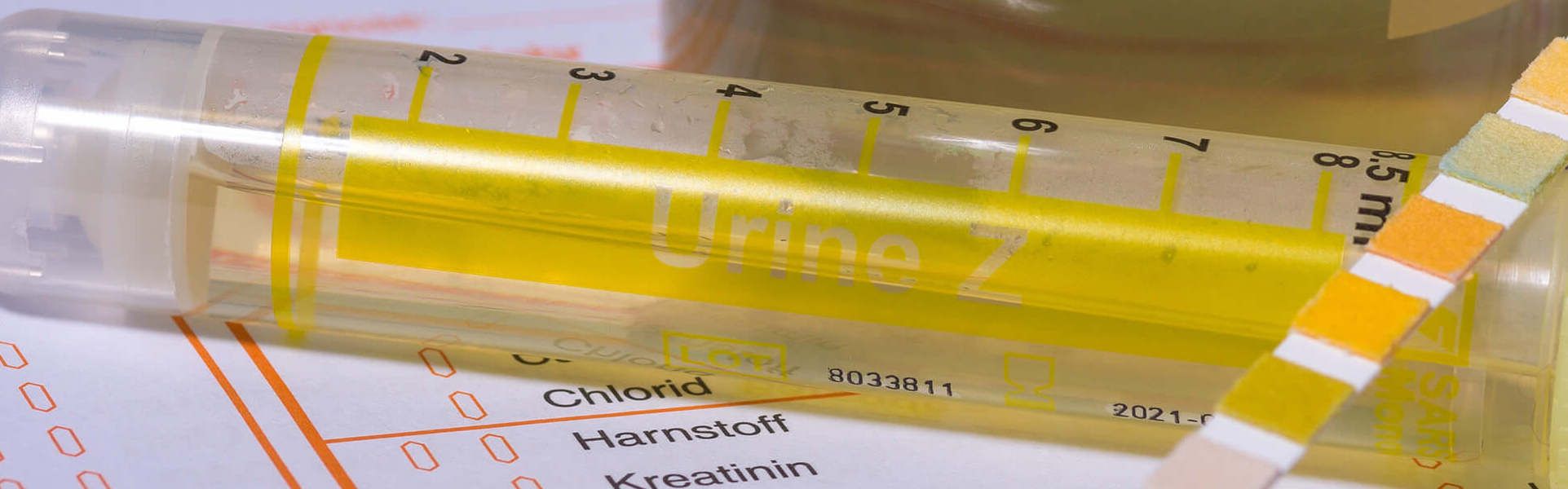
The Hamburg Glomerulonephritis Registry was set up as part of the Collaborative Research Center 1192 (SFB 1192) at the University Medical Center Hamburg-Eppendorf. It is a data- and biobank which collects selected clinical data and biomaterials from patients with immune-mediated glomerular diseases (glomerulonephritis). These data and biomaterials (blood, urine, and kidney tissue samples) are used for research purposes by the scientists of the Collaborative Research Center.
What are the goals of the Hamburg Glomerulonephritis Registry?
The Hamburg Glomerulonephritis Registry helps to advance the research of immune-mediated glomerular diseases.
The biomaterials and selected clinical data collected at the time of the diagnosis and during a follow-up enables the researchers to investigate the exact mechanisms leading to the onset and progression of the disease and find new therapeutic options.
For this purpose, the investigation of a sufficiently large number of patients is imperative, which is why the registry was implemented as a central infrastructure of the Collaborative Research Center.
Which diseases are being investigated?
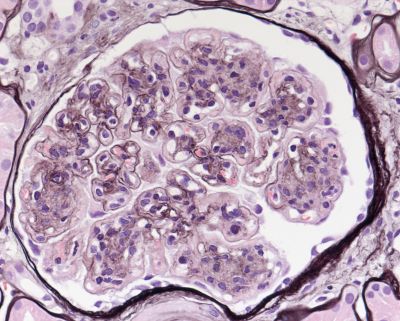
Glomerulonephritis represents a group of kidney diseases, in which inflammatory processes in the glomeruli play a central role. Often these diseases lead to a deterioration of kidney function and kidney failure. There are diverse forms of glomerulonephritis with different prognosis and treatment options. In order to identify the exact cause, or underlying disease in a patient usually a kidney tissue sample (kidney biopsy) is needed.
In order to better understand how a glomerulonephritis form develops and progresses, the examination of material from patients with this disease is pivotal. Therefore, the contribution of patients with biosamples (i.e. blood samples) by participating in the registry is of outmost importance in order to reach our goal of finding new therapeutic options for these diseases.
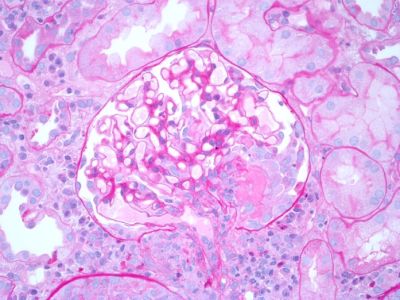
Membranous nephropathy is a kidney disease characterized by severe protein loss in the urine and swelling of the limbs due to water retention. These characteristic clinical symptoms are called nephrotic syndrome.
Membranous nephropathy is caused by binding of proteins (antibodies) on specific cells in the glomeruli, called podocytes. In up to 85% of patients two antibodies are responsible for the development of disease and can be detected in the blood (PLA2R1- and THSD7A-antibodies). Which other antibodies may cause membranous nephropathy, how these antibodies develop and how do they damage the kidney are some key aspects investigated by various research groups in the Collaborative Research Center.
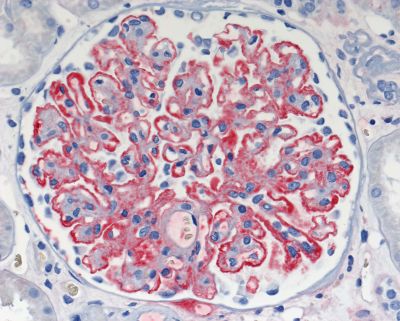
The inflammation of small vessels (vasculitis) is the hallmark of ANCA-associated vasculitis. This is a systemic disease, which can affect different organs. When the kidneys are affected, it is called ANCA-associated glomerulonephritis. ANCA-associated vasculitis may present as: granulomatosis with polyangiitis (GPA, formerly Wegner's granulomatosis), microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (eGPA, formerly Churg-Strauss syndrome). Often the disease shows a very aggressive course with a rapidly progressive deterioration of kidney function and is called rapidly progressive glomerulonephritis (RPGN). Since the migration of inflammatory cells into the glomeruli of the kidneys is one of the histologic hallmarks of the disease, different research groups of the Collaborative Research Center investigate this process in more detail. Furthermore, some research groups of the Collaborative Research Center are implementing novel technologies to analyse molecules in the blood, which play a role in inflammation and may serve as possible new targets of therapy.
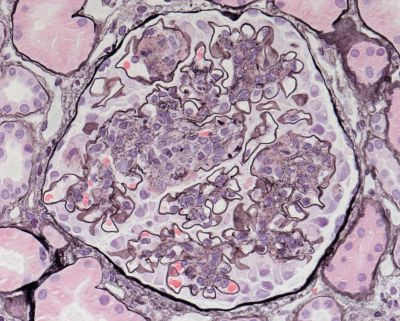
This disease is characterized by scaring of the smallest filtration units of the kidney (glomeruli). FSGS does not represent one single disease entity, but rather a description of the kidney microscopic appearance of different diseases. The causes for these changes in the kidney range from genetic causes to toxic damage. The investigation of the underlying molecular mechanisms is an essential goal of our Collaborative Research Center.
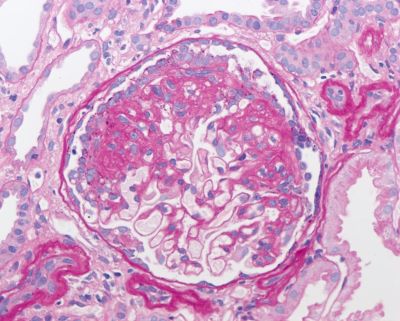
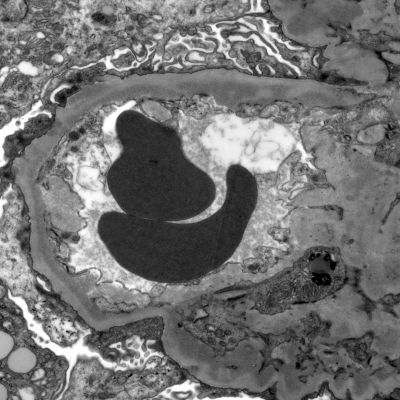
The clinical hallmark of minimal change disease is a nephrotic syndrome with severe loss of protein in the urine. Interestingly, no abnormalities can be depicted in light microscopic examination of kidney tissue (kidney biopsy). Only at very high scale magnification in electron microscopic pictures changes in the filter units of the kidney can be detected.
Membranoproliferative glomerulonephritis is a rare kidney disease, which is often caused by infections (i.e. Hepatitis C), dysregulations of the immune system, etc. In some cases, the disease is mediated by dysregulation of the complement system and is called C3 glomerulopathy. In this case, components of the complement system, i.e. complement C3, are deposited in and lead to inflammation of the glomeruli. Detailed investigations of the mechanisms how these diseases develop (i.e. the role of mutations in specific complement genes) is the subject of some projects in the Collaborative Research Center.
Systemic lupus erythematosus (SLE) is one of the more common autoimmune diseases. The disease is characterized by an inflammatory reaction against the body's own tissue. The causes leading to disease development are mostly unclear. SLE can affect many different organs. If the kidneys are affected, it is called lupus nephritis. The investigation of the mechanisms how this disease develops and identification of molecules influencing disease progression are the subject of research by some groups of the Collaborative Research Center.
There are other rare forms of glomerulonephritis, such as the anti-GBM nephritis. In this form of disease, proteins (antibodies) are formed, which lead to inflammation of the glomeruli and the lung. In order to investigate these rare forms of glomerulonephritis and to uncover basic mechanisms of disease development, the study of large patient cohorts is needed. For this purpose, the Hamburg Glomerulonephritis Registry was implemented.

How does participation in the registry work?
For the correct diagnosis of an immune-mediated glomerular disease, usually examinations of blood, urine and kidney tissue (kidney biopsy) are needed. These examinations take place independently of the participation in the registry and are crucial for the correct diagnosis of the disease. Material which is no longer needed for the diagnosis and treatment can be scientifically used in the Hamburg Glomerulonephritits Registry if the patient has given his/her consent. In addition, selected clinical data are recorded.
Contact
Do you have any questions or would you like support the scientific progress in the field of immune-mediated glomerular diseases? Feel free to contact us or your nephrologist.
Hamburg Glomerulonephritis Registry
Contact: PD Dr. Elion Hoxha
Universitätsklinikum Hamburg-Eppendorf
Zentrum für Innere Medizin
III. Medizinische Klinik und Poliklinik
Martinistraße 52
20251 Hamburg
Telefon: +49 (0) 40 7410-58817
Fax: +49 (0) 40 7410-49017
Email: This email address is being protected from spambots. You need JavaScript enabled to view it.

